The Human Sciences Research Council (HSRC) released the key findings of the Sixth South African HIV Prevalence, Incidence, and Behaviour Survey (SABSSM VI) at a satellite session held at the 2024 International AIDS Conference on 24 July 2024.
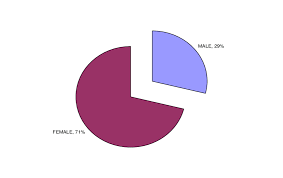
The survey found that HIV prevalence for all ages decreased from 14.0% in 2017 to 12.7% in 2022 translating to a decline from 7.9 million (2017) to 7.8 million (2022) people living with HIV. However, the data shows that females continue to be disproportionately affected by HIV with a prevalence of 16.4% as compared to males at 8.8% of all ages. Prevalence peaks at 34.2% for females aged 35–39 years, whereas, prevalence peaks at 27.1% for males aged 45–49 years.
HIV incidence in people aged two years and older in 2022 was 0.44%, translating to 232 400 new HIV infections in South Africa. HIV incidence was 0.60% among adults 15 years and older translating to 227 400; 0.39% among youth and young adults aged 15–24; and 0.72% among adults aged 15–49 years. In 2022, the HIV incidence rate was consistently higher in females than males in all age categories.
In terms of treatment, South Africa recorded an increase in antiretroviral treatment (ART) coverage, from 63.7% in 2017 to 80.9% in 2022. This translates to an estimated 5 700 000 people living with HIV receiving ART, an increase from 4 500 000 in 2017. A greater proportion of females, 83.2% than males, 76.2% were on ART. HIV viral load suppression stands at 81.4% for all ages.
The SABSSM VI survey, conducted between 2022 and 2023, aimed to maintain surveillance of HIV infection and behaviours in South Africa, evaluate the progress of the South African national HIV and AIDS, STI and TB Strategic Plan, and monitor HIV indicators for national and international reporting.
The survey’s key objectives included estimating HIV prevalence and incidence, viral load suppression, and exposure to HIV-related services among adults and children. It also assessed progress towards the 2030 UNAIDS 95-95-95 targets, HIV drug resistance, and the relationship between social and behavioural factors, intimate partner violence, and HIV infection.
Progress towards the 95-95-95 targets improved, with 89.6% of people living with HIV knowing their status, and of those knowing their status, 90.7% on treatment, with 93.9% of those who knew their status and being on treatment being virally suppressed. Improvement across the 95-95-95 indicators was more pronounced in males compared to females. Overall, the survey found 81.4% of all people living with HIV were virally suppressed.
However, it is concerning that the survey further reveals that gaps remain in knowledge of HIV status among youth aged 15-24 (73.1%). Early sexual debut, age-disparate relationships, multiple sexual partners, and low condom use persist as key drivers of HIV. Awareness and uptake of pre-exposure prophylaxis (PrEP) are increasing.
According to the overall principal Investigator of the study, HSRC’s Prof Khangelani Zuma, HIV-related stigma remains a significant issue among people aged 15 years and older. “Addressing stigma is essential to improving the quality of life and well-being of people living with HIV. However, of the six questions related to HIV-related stigma, the majority yielded results that indicated that most people held positive attitudes toward people living with HIV,” said Prof Zuma.
The survey achieved a household response rate of 80% and an individual interview response rate of 94.1%. A total of 47,766 participants provided blood specimens for HIV testing, resulting in a testing response rate of 62.7%.
Prof Zuma indicated that the results suggest advancements in the fight against the HIV epidemic in South Africa. “This is evidenced by a stabilisation of HIV prevalence, ageing epidemic, a reduction in HIV incidence, enhancements in HIV treatment outcomes such as increased rates of ART coverage and viral load suppression (VLS) in line with the 95-95-95 targets,” added Prof Zuma.
The survey recommends key actions that can address the HIV epidemic as a public health threat in South Africa by 2030. These include continuing intensive programme focusing on reducing new infections among adolescent girls and young women. It also recommended enhancement of prevention efforts that target groups disproportionately affected by the drivers of HIV infection such as women and young people.
The survey was conducted by the HSRC in partnership with the US Centers for Disease Control and Prevention (CDC), South African Medical Research Council (SAMRC), the University of Cape Town (UCT), and the National Institute for Communicable Diseases (NICD).
Click on the link below to download full report, presentation, and 20 year anniversary video:
https://hsrc.ac.za/special-projects/sabssm-survey-series/sabssm-vi-media-pack-july-2024/
Ends.
For media enquiries:
Adziliwi Nematandani
Cell: +27 82 765 9191
Email: anematandani@hsrc.ac.za
Join the conversation:
AIDS2024
HIV
AIDS
Notes to the editor
About the Human Sciences Research Council (HSRC)
The HSRC was established in 1968 as South Africa’s statutory research agency and has grown to become the largest dedicated research institute in the social sciences and humanities on the African continent, doing cutting-edge public research in areas that are crucial to development.
Our mandate is to inform the effective formulation and monitoring of government policy; to evaluate policy implementation; to stimulate public debate through the effective dissemination of research-based data and fact-based research results; to foster research collaboration; and to help build research capacity and infrastructure for the human sciences.
The Council conducts large-scale, policy-relevant, social-scientific research for public sector users, non-governmental organisations and international development agencies. Research activities and structures are closely aligned with South Africa’s national development priorities.